Case Report Download PDF
Pott’s disease - The Under diagnosis Prevalence and Its Severe Repercussions
Received: October 11, 2019 Published: October 21, 2019
Abstract
A senile male with back pain, fever, weight loss and a tuberculin skin test positive, was treated for bacterial spine abscess for many times without improvement of symptoms. Lately, after a large period of neurological complaints, antituberculosis treatment was initiated empirically. Currently, the patient has been treated on an outpatient basis without fully improving his health, persisting with some sequalae. A difficulty to come up with the diagnostic of Pott Disease has justified the extensive propaedeutic used, besides ineffective results of the first treatments instituted and less objectivity in the conduction of the case.
Introduction
According to the World Health Organization, tuberculosis is one of the main causes of death among the infectious diseases, with approximately 1.8 million of deaths per year. Among the different forms of the disease, the musculoskeletal form corresponds to up to 3% of all cases, and the vertebral tuberculosis is responsible for half of them. Therefore, neurological associated manifestations are responsible for high morbidity of the disease (VILAR et al. 2006). Pott’s disease (PD) is a manifestation of the extra pulmonary tuberculosis that affects the spine. It’s a neglected and under diagnosed disease and it is often approached lately. Its triad includes gibbosity, abscess and paraplegia, being the chronical back pain highly suggestive [1]. The most affected place is the thoracic spine, followed by the lumbosacral and cervical spines, with 50%, 40% and 10% of the cases diagnosed, respectively
In this manuscript, the authors aim to report a case of one male patient with vertebral tuberculosis, presenting with painful lump in the lower back, which was not early properly diagnosed, generating clinical manifestations for over a year. In addition, a brief literature review was performed focusing on the diagnosis and treatment of the bone tuberculosis.
Case Report
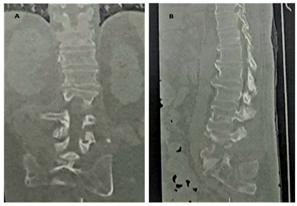
A male patient with 66 years-old, diabetic, paraplegic 24 years ago due to automotive trampling, with a past history of recurrent urinary tract infection, presents a constant low back pain for over a year ago, 10/10 in intensity, radiating down to sacral area, that improves partially with tramadol, and evolving with lower back bulging and intermittent fever. Furthermore, he presented nausea, hyporexia, chills and loss of 15 Kg in 9 months. He was in a good general condition, oriented, with reduced vesicular murmur at the pulmonary apex and abolished at the basis, owning resonant percussion note of the entire chest. Lumbosacral computed tomography evidenced expansive osteolytic injury (L5-S1) with destruction of the intervertebral disc and modifications in adjacent soft tissues (Figure 1). A tuberculin skin test was positive: 15 mm. Besides the bone lesions, there was an associated diagnosis of paravertebral abscess and spondylodiscitis, for which had already been used antibiotic therapy (Ceftriaxone, Oxacillin, Vancomycin and Cefepime), and the patient had undergone three surgical procedures debride and remove the lumbosacral nodule. Even without previous pulmonary involvement, a therapeutic test with Gabapentin, Rifampicin, Isoniazid, Pyrazinamide and Ethambutol was performed. The patient latter evolved with poor improvement, being readmitted to hospital care to use Polymyxin B, Tigecycline and Amikacin empirically. In continuity, the patient still presented several hospitalizations due to neurological symptoms and back pain. Currently, he is on an outpatient care without fully improving his complaints.
Figure 1: Computed tomography of lumbar and sacral spine demonstrating expansive osteolytic injury (L5-S1) with destruction of the intervertebral disc. A) Coronal view. B) Sagittal view.
Discussion
Pott’s disease (PD) is a common manifestation of extrapulmonary tuberculosis in which there is spine involvement (WEBER et al., 2009). At about 10% of extrapulmonary tuberculosis has bone involvement and the spine is the main site affected, which makes up 1 to 2% of the total cases of tuberculosis [2]. PD occurs through the reactivation of a foci from hematogenous or lymphatic dissemination which metastasize to the spine, affecting preferably weight bearing joints and bones (VEIGA, 2009). These lesions present clinical manifestations more frequently in at risk population as debilitated chronic patient, immunosuppressed or immunocompromised, HIV seropositive individuals, previous spine surgery, use of corticosteroids and/or intravenous drugs, and kidney or liver insufficiency. Foci reactivation can be premature or after years from the primary infection [1]. The most common symptom is chronic dorsal pain, besides the localized bulging presentation and other deformities, like kyphosis. Worsening factors are movement, cough, weightlifting and local percussion. The main constitutional symptoms include fever, weight loss, weakness, night sweating and body aches [1]. Regarding the neurological impairment, it is reported since loss of muscle strength and progressive limbs hypoesthesia to spastic paraplegia or quadriplegia with symmetric hyper reflexia. Bladder retention and sphincter modifications at compatible sensory levels, spinal compression, as well as root pain, numbness and weakness may occur [1].
Even with its severity and clinical relevance, vertebral tuberculosis is still a neglected disease in research and therapeutic fields, possibly due to the fact that it affects low income people [3]. Furthermore, the disease’s under diagnosis is responsible for often irreversible sequelae. Therefore, it is the most severe form of the bone tuberculosis, being necessary the adoption of measures that aim to interrupt the progression of the disease and consequently the spinal destruction and deformity, as well as the neurologic symptoms like paraplegia. Late diagnosis is common, since that many times the disease has a non-specific symptomatology and also because of the absence of a pulmonary disease ongoing concomitantly. The average delay is approximately six months [4]. Clinical clues at anamnesis that suggest PD must contemplate previous close contact with people with tuberculosis or places that are endemic areas for this disease, besides chronic thoracolumbar pain, especially in children [5].
The gold standard for PD diagnosis is magnetic nuclear resonance associated with computed tomography (CT)-guided biopsy, followed by sample cultivation [1]. In medical practice, CT is more accessible and when it shows a focus of calcification within the abscess it is practically pathognomonic of bone tuberculosis [6]. There are several differential diagnoses which corroborates to the under diagnosis, and there are still many controversies regarding the therapy, especially with respect to its duration and the inclusion of adjuvant surgical treatment.
Concerning the treatment, it may be conservative or surgical, depending on the nature of the case and also on the available orthopedic or neurosurgical facilities [7]. Conservative treatment is based on rest, spine stabilization, and administration of anti-tuberculosis chemotherapy. For specific drug therapy, the Brazilian Ministry of Health advises that the use of Rifampicin, Isoniazid, Pyrazinamideand Ethambutol should be instituted for 2 months, keeping Rifampicin and Isoniazid for another 10 months [8,9]. On the other hand, the surgical method pursuits to: perform aspiration or drainage of cold para vertebral abscesses, promoting earlier regression of the infectious process, in addition to decompressing noble structures; accomplish mechanical debridement of the necrotic focus as a more conservative technique, acting only on necrotic tissues; promote decompression of neural structures and stabilization of the spine in cases of short-term paraplegia (<6 months), allowing the recovery of neurological deficits; and fixate the spine in cases of kyphosis with spinal instability or large angulation. (VILAR et al. 2006).
In the face of this scenario, it is clear that Pott's disease is still an under diagnosed disease due to low suspicion in health services, either because it is poorly investigated nowadays, or because of its peculiar clinical aspect as it presents itself as an insidious condition with chronic symptomatology and progression, without pathognomonic signs of the infection. Although rare studies add something to the differential diagnosis, they do little to solve the collusion on the duration of clinical treatment and the best surgical technique used in the disease. On the contrary, they bring only more possibilities for treatment and no innovation in these protocols, which generate more controversy. Thus, PD should be the subject of further study after all it is not such an uncommon disease as it seems to most people.
This singular condition of PD, coupled with low clinical suspicion, management by various patient care services, little appreciation of initial constitutional symptoms, and occasional finding of comorbidities, made difficult the diagnostic definition and justified the extensive propaedeutic used, following ineffective results of the first treatments instituted and less objectivity in the conduction of the case.
Acknowledgment
The authors thank to medical corps of Hospital GiseldaTrigueiro and to the patient, who allowed the story of his case.
References
- Mello MCP, Silva FBB, Ehendo KMS, Botura RI, Gonsaga RAT (2014) Mal de Pott: uma revisão bibliográfica dos últimos 5anos / Pott's Disease: a bibliographic review from the last 5 years. Com. Ciências Saúde 25(2): 173-184.
- Basta PC, Marques M, Oliveira RL, Cunha EAT, Resendes APC, et al. (2013) Desigualdades sociais e tuberculose: análise segundo raça/cor, Mato Grosso do Sul. Rev Saúde Pública 47(5): 854-864.
- McAdam AJ, Sharpe AH (2010) Doenças Infecciosas. In: Kumar V, Abbas AK, Fausto N,Aster JC (Eds). Robbins&Cotran- Patologia: Bases Patológicas das Doenças (8th edn). Elsevier. São Paulo. pp. 368-375
- Kamara E, Mehta S, Brust JCM, Jain AK (2012) Effect of delayed diagnosis on severity of Pott’s disease. IntOrthop 36(2): 245-254.
- Masavkar S, Shanbag P, Inamdar P (2012) Pott’s spine with bilateral psoas abscesses. Case Rep Orthop 2012: 208946.
- Griffth JF, Kumta SM, Leung PC, Cheng JCY, Chow LTC, et al. (2002) Imaging of Musculoskeletal Tuberculosis: A New Look at an Old Disease. Clin Orthop Relat Res 398: 32-39.
- Toledo JRACC, Greco DB, Figueiredo CM (2000) Risk factors for tuberculosis among HIV-infected persons. A case-control study in Belo Horizonte, Minas Gerais, Brazil. Mem Inst Oswaldo Cruz 95(4): 437-443.
- Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Vigilância das Doenças Transmissíveis. Manual de Recomendações para o Controle da Tuberculose no Brasil / Ministério da Saúde, Secretaria de Vigilância em Saúde, Departamento de Vigilância das Doenças Transmissíveis. – Brasília: Ministério da Saúde, 2019.364 p
- Garg RK, Somvanshi DS (2011). Spinal tuberculosis: a review. J Spinal Cord Med 34(5): 440-454.